The Fundamentals Of HPV And Cervical Cancer
By the age of 50, 80% of women will have been infected with human papillomavirus (HPV)[1]. For most, the virus, which exists in more than 100 types, will clear up without any treatment. But an HPV genotype 16 and 18 infection puts women at risk of developing cervical cancer[2]. that can be fatal if not detected/managed in time. To simplify the fundamentals, here’s what a woman should know about the HPV virus and cervical cancer.
What you can do if your screening reveals you have a high risk HPV infection
It can be shocking and distressing to hear the news. Step one, discuss the findings of the HPV test with your doctor in more detail. You may be referred to gynaecological outpatient care, which may mean an additional test or undergoing a colposcopy. This procedure allows the gynaecologist to examine your cervix more closely and take a small amount of tissue for further analysis if there appear to be any abnormalities. There is also a possibility of the taking a small amount of the tissue, should the gynaecologist see any signs of pre-cancer or early cancer.
Interpreting the screening
The aim of HPV screening aims to provide information to protect women’s health. To start with, talk to your doctor to figure out if the genotype is HPV is 16 or 18 or any other high-risk genotype. Ask the gynecologist for more information on risk of cancer. The HPV is transmitted sexually, usually from a man to woman, and the course of the infection may differ according to your age. The infection could be short-lived and clear quickly with younger women. If you are diagnosed with HPV at an older age, persistent infection with a much higher pre-cancer risk is more likely. [3]
Another aspect to keep in mind is that most people get infected with just one genotype, but some have a mixed genotype-that is more than one genotype infection.
After the initial positive test results, you would possibly need to be re-tested about 12 to 18 months later. Re-testing is likely to continue until cleaning up the virus or removal of abnormal lesions is complete. A high-risk HPV infection means having several years of involvement with the health care system.
The conversation with the partner
If your partner is a male, the risk of developing penile cancer is higher[4]. If your partner is a woman, the risk of infection and cervical cancer is high. Those involved with multiple partners should also be aware of a higher associated risk for HPV infection[5].
A timeline view: High-risk infections transforming into cervical cancers
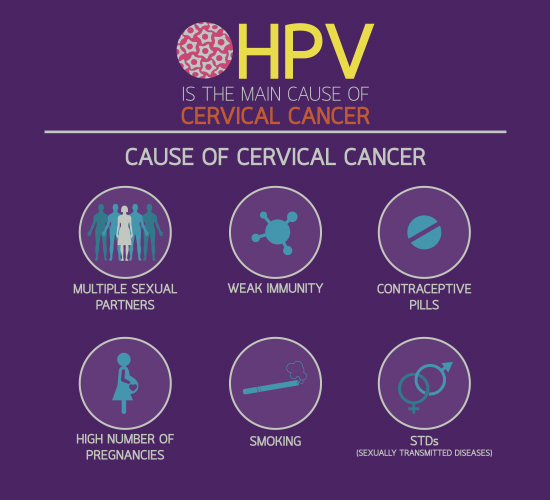
Just 2 to 4% of high-risk infections cause clinically significant lesions. Nevertheless, the risk is greater if your HPV infection continues. Testing HPV is a ‘risk test’. If the test is negative, there is a 90-95% probability that you will not develop cervical cancer[6]. Even if there is a infection with a high-risk genotype, it may take 10-15 years to transform into cervical cancer. However, a compromised immune system, lymphoma or leukaemia could potentially speed up the development of cervical cancer. Having multiple sexual partners or being infected with HIV or other sexually transmitted diseases (STDs) may also contribute to a quicker conversion to cervical cancer. Early-age sexual activity, herpes, syphilis, lifestyle factors such as smoking etc. are other factors that may speed up the chance of developing cervical cancer[7].
The Virus Vs Your Fertility
If you have HPV and other STDs, you can develop inflammatory pelvic disease which may affect fertility. HPV has no effect on pregnancy . You don’t pass the HPV infection on to your unborn child when you are pregnant.
However, if you are infected with the low-risk HPV genotypes 6 and 11 during childbirth, you may be able to transmit the virus to the baby in the birth channel, which could lead to a condition known as recurrent respiratory papillomatosis or RRP. If this happens, it could affect your child’s larynx.
References:
-
- Chesson HW et al. Sex Transm Dis. 2014;41(11):660-664: https://pubmed.ncbi.nlm.nih.gov/25299412/
- De Sanjose S et al. Lancet Oncol. 2010: https://pubmed.ncbi.nlm.nih.gov/20952254/
- Blanks RG et al. BJ of Cancer 2009; 100(11): 1832 – 1836:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695690/
- https://www.cancer.org/cancer/penile-cancer/causes-risks-prevention/risk-factors.html
- http://www.who.int/mediacentre/factsheets/fs380/en/
- https://www.cancer.gov/news-events/press-releases/2014/HPVscreeningPredictor
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1769629/